As the COVID pandemic has put tremendous financial pressure on skilled nursing facilities, nursing homes, and LTC facilities, the ability to maximize profits and improve efficiencies has never been more crucial.
A primary opportunity for facilities and operators to make a significant impact on their bottom line is by ensuring they are receiving the maximum eligible rebates on their drug spend each month. These rebates can add up to hundreds of thousands, if not millions of dollars, for operators depending on the number of facilities they own.
Without the right processes and technologies in place, you could be missing out on millions in rebates delivered back to your facilities each year. Figuring out just how to maximize these rebate dollars, however, is much more complex than simply sending a claim to a manufacturer. The following are 4 ways to ensure that you get the most from your rebate dollars and reach the lowest net cost on your pharmacy spend.
Drug Utilization Management
All LTC facilities should have an approved formulary–a list of preferred medications that guide clinicians in prescribing drugs for residents and patients–as part of an effective drug utilization management practice. Formularies must balance clinical outcomes and patient needs with financial considerations. One way to maximize rebates is to select therapeutically-equivalent drug alternatives that offer competitive manufacturer rebates. The more alternatives a facility can identify that meet the determined balance of needs, the more savings the facility will be able to enjoy.
SRX has advisors and registered pharmacists who are able to work with your team to develop a formulary that meets the needs of your patient population while also improving your profitability. This allows operators to invest more into their facilities, personnel, and better patient experiences to improve competitiveness in the market. Paula Agoglia, a licensed registered pharmacist and SRX’s SVP of Business Development, advises customers on their drug utilization management. With over 20 years of experience in the LTC industry and pharmacy cost containment, she understands the importance of this process for operators. “A well-planned and managed formulary is the foundation of a successfully managed pharmacy practice. Done properly, it provides the guidelines needed to ensure that the clinical side of your operations is aligned with the financial side of your operations and vice versa. Just making sure this alignment is part of your operational strategy is an important step not only in obtaining important rebate dollars, but also reducing waste and improving other efficiencies.”
Automation
Once you have a formulary established, the next step is putting measures in place that enforce the drug utilization. Without the aid of technology and automation, it is quite common that drug utilization rules are broken either on the clinical side or by the pharmacy partner. To avoid this, facilities can implement point-of-sale adjudication, an automated process that builds all your formulary rules along with your pharmacy contract terms into software that manages your pharmacy relationship. When adjudication is possible, clinicians are unable to prescribe, and pharmacies are unable to fill, off-formulary medications. The ability to control the selection of drugs is another critical step toward ensuring your ability to maximize rebate dollars.
When point-of-sale adjudication is not possible, often due to the capabilities and willingness of existing partner pharmacies to participate, a drug utilization review (DUR) can provide a detailed report of all claims, including off-formulary prescriptions that may have been filled. With this report, facilities can easily request credits and returns from their pharmacy partners, as well as identify prescriptions that have been combined or coded in a way that may hide eligible rebates.
Erik Reaveley, a Principal and Chief Strategy Officer at SRX, was instrumental in developing SRX’s DUR process. He explains, “One of the main challenges we saw when we began looking at solutions to help LTC operators manage their pharmacy spend was in the area of reviewing claims. A lot of operators still do this manually. We are talking about thousands of line items – that’s not efficient. By automating this review process, we can provide a level of insight not available anywhere else on the market. For clients not currently able to adjudicate, our reports are an invaluable tool in capturing rebates, as well as returns and credits that often go unnoticed if they have to be identified manually.”
Right Partner, Right Solution
Managing the complexity involved in pharmacy spend requires a broad base of industry knowledge in order to fully understand how to minimize drug costs and get the highest number of rebates. The right technology partner, with solutions for automation, reconciliation and reporting can keep your facility on track for realizing the lowest net cost on your pharmacy spend. At SRX, we have a wealth of industry experts who provide the support you need to leverage our technology to significantly impact your bottom line. We guarantee our quarterly rebate payments, and insist on a timely reimbursement schedule for every client, every time.
Scott Taylor, CEO explains, “Operators have a lot on their plates, especially now. Our mission is to provide solutions that reduce their burdens through automation, technology, and advisory support. Our customers see us as a valued partner in their cost savings strategy, but a big piece of that is the check they get each quarter. Money talks. Those are important dollars that can be used elsewhere.”
Expect Results
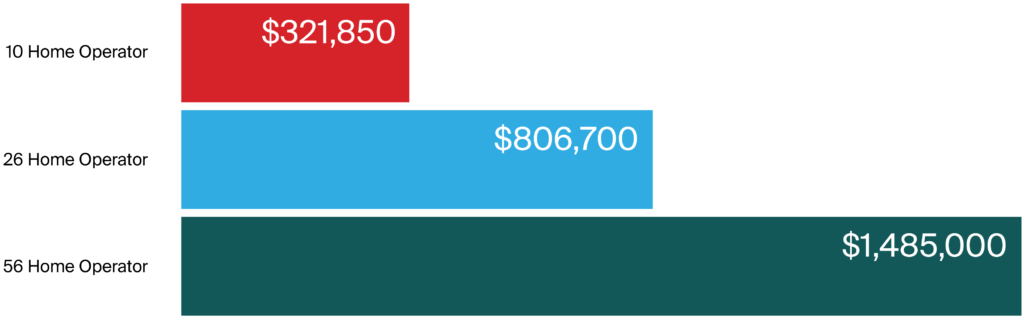
When operators employ the right strategies to manage their pharmacy spend they can expect to see significant results. Our clients range from small operators to some of the largest in the industry. Results vary based on the number of facilities, patient mix, and other factors, but in each case our customers have been surprised by the increase in the rebates they have received with our solution. The following are actual rebate dollars we were able to capture for our clients in 2020:
If you would like to learn more, we offer a free rebate calculator that estimates the rebate dollars your facility may be eligible for by using our solution. Contact us today to schedule a demo or speak with one of our experts.
SRX is a technology and advisory company that helps LTC operators realize the lowest net cost on pharmacy spend. We help our customers improve drug utilization, manage pharmacy relationships, reduce costs and waste, and maximize rebates. We are committed to transparency and accountability and guarantee our quarterly rebates are paid on time, every time. Contact us at 833 633 6833.
Learn more about our rebate services.